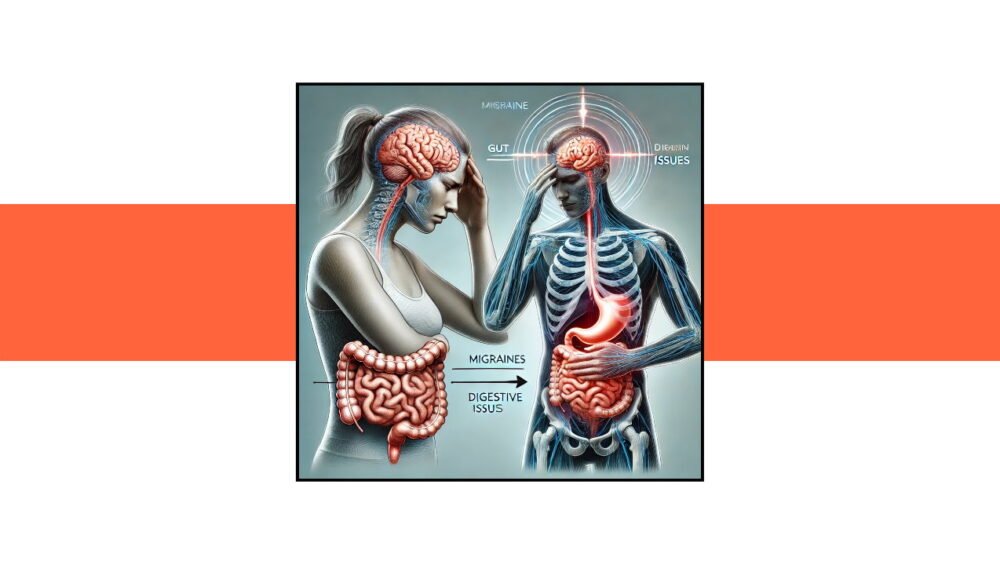
Have you ever experienced a migraine that seems to come out of nowhere, leaving you debilitated and struggling to function? Now, imagine coupling that intense head pain with an unexpected wave of digestive issues. This perplexing combination of symptoms can leave anyone feeling desperate for answers. Welcome to the lesser-known world of migraine-related digestive disturbances, a connection that often goes unnoticed but can significantly impact your overall well-being.
In this blog, we’ll embark on a journey to uncover the intricate relationship between migraines and digestive health. By the end, you’ll have a deeper understanding of how these two seemingly separate issues are intertwined and, more importantly, what you can do to manage them effectively.
The Migraine-Digestive Connection: An Overview
Migraines are often dismissed as “just a headache,” but they are far more complex. These neurological events can cause severe pain, visual disturbances, and even sensory sensitivities. However, the connection between migraines and the digestive system is less understood but equally significant.
Why the Digestive System?
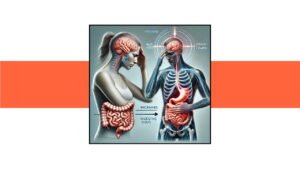
The gut-brain axis is a bidirectional communication system linking the central nervous system (brain) and the enteric nervous system (gut). This connection explains why digestive disturbances can coincide with migraines. When your brain experiences the turmoil of a migraine, it can send distress signals to your gut, leading to symptoms like nausea, vomiting, diarrhea, and abdominal pain. Conversely, gastrointestinal issues can trigger or exacerbate migraines, creating a vicious cycle that is hard to break.
Understanding the Mechanisms
To grasp why migraines and digestive issues often occur together, it’s essential to delve into the underlying mechanisms:
Neurotransmitters
Serotonin, a key neurotransmitter, plays a crucial role in both migraines and digestive health. During a migraine, serotonin levels fluctuate, which can disrupt gut motility and sensitivity. This can result in nausea, vomiting, and diarrhea.
Inflammation
Migraines and certain digestive disorders share common inflammatory pathways. Pro-inflammatory cytokines can be released during a migraine, leading to inflammation in both the brain and the gut. This inflammation can exacerbate gastrointestinal symptoms and contribute to the overall misery of a migraine attack.
Autonomic Nervous System
The autonomic nervous system regulates involuntary bodily functions, including digestion. During a migraine, this system can become dysregulated, leading to issues like delayed gastric emptying (gastroparesis) and increased gut sensitivity.
The Role of Diet and Lifestyle
Diet and lifestyle choices can significantly impact both migraines and digestive health. Understanding the triggers and implementing changes can help manage these conditions more effectively.
Common Triggers
- Food Sensitivities: Certain foods, such as chocolate, caffeine, alcohol, and processed foods, can trigger migraines and digestive issues.
- Hydration: Dehydration is a well-known migraine trigger and can also cause constipation and other digestive disturbances.
- Stress: Chronic stress can exacerbate both migraines and gastrointestinal problems. Managing stress through techniques like meditation, yoga, and regular exercise is crucial.
- Sleep: Poor sleep quality can trigger migraines and disrupt digestive function. Establishing a consistent sleep routine can help mitigate these issues.
Diagnosis and Management
If you suspect that your migraines and digestive issues are connected, it’s essential to seek medical advice. A comprehensive approach can help identify triggers and manage symptoms more effectively.
Medical Evaluation
- Detailed History: Your healthcare provider will take a thorough history of your symptoms, including the frequency and severity of migraines and digestive issues.
- Diagnostic Tests: Tests such as blood work, imaging studies, and gastrointestinal evaluations may be necessary to rule out other conditions and confirm the diagnosis.
Treatment Options
- Medications: Prescription medications, including triptans for migraines and antispasmodics for digestive issues, can provide relief.
- Dietary Changes: Working with a nutritionist to identify and eliminate trigger foods can significantly reduce symptoms.
- Lifestyle Modifications: Incorporating stress management techniques, regular exercise, and proper hydration can help manage both conditions.
- Probiotics: These beneficial bacteria can help maintain gut health and may reduce the frequency and severity of migraines.
Case Study: Sarah’s Journey
To illustrate the connection between migraines and digestive health, let’s look at Sarah’s experience.
Sarah, a 35-year-old professional, had been suffering from migraines for over a decade. Recently, she noticed that her migraine attacks were often accompanied by severe nausea and diarrhea. Frustrated, she consulted her healthcare provider, who suggested a comprehensive approach to manage her symptoms.
Through dietary changes, Sarah identified that dairy and processed foods were significant triggers. By eliminating these from her diet, she experienced a dramatic reduction in both migraine frequency and digestive disturbances. Additionally, incorporating stress management techniques and maintaining proper hydration helped her manage her symptoms more effectively.
Sarah’s journey highlights the importance of understanding the migraine-digestive connection and adopting a holistic approach to treatment.
Conclusion
The relationship between migraines and digestive health is complex but undeniable. By recognizing this connection, you can take proactive steps to manage both conditions effectively. Remember, it’s not just about treating the symptoms but understanding the underlying mechanisms and making lifestyle changes that support overall health.
If you suffer from migraines and digestive issues, don’t hesitate to seek medical advice. With the right approach, you can break the cycle and improve your quality of life. Stay informed, stay proactive, and take control of your health journey.