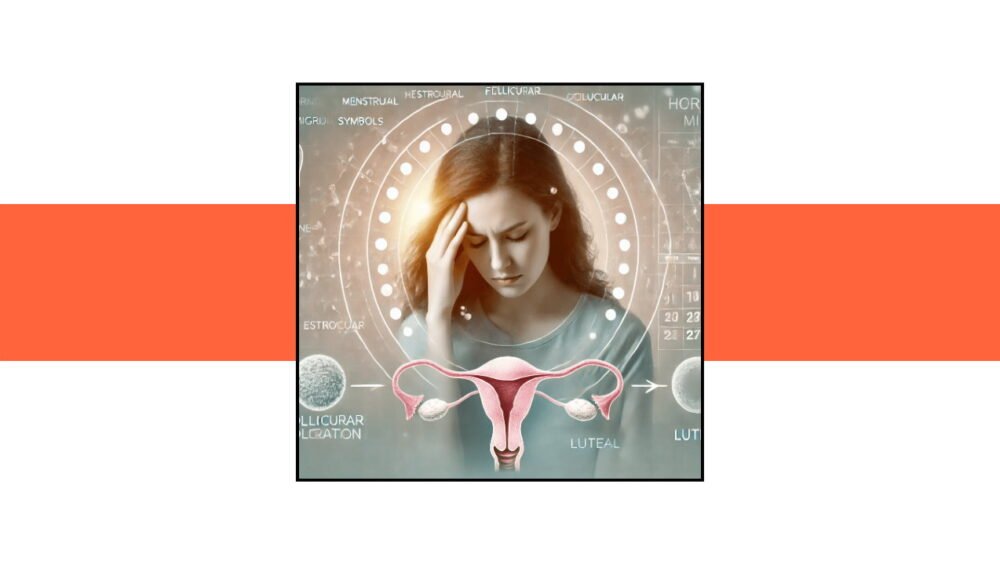
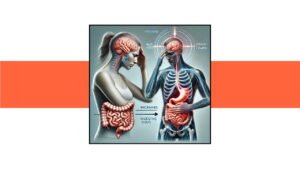
Migraines are more than just headaches; they are debilitating experiences that can significantly disrupt daily life. Among the various types of migraines, hormonal migraines are particularly enigmatic. Despite affecting millions of people, primarily women, their underlying mechanisms are not well understood. This lack of understanding leaves a critical knowledge gap that we aim to fill in this comprehensive guide. So, what exactly are hormonal migraines, and why do they occur? Let’s embark on a journey to unravel this mystery and provide you with the information you need to better understand and manage this condition.
What Are Hormonal Migraines?
Hormonal migraines, as the name suggests, are migraines that are closely linked to hormonal fluctuations in the body. These migraines are most commonly associated with the menstrual cycle, but they can also be influenced by other hormonal changes such as pregnancy, menopause, and even hormonal contraceptive use.
The Role of Estrogen
One of the key players in hormonal migraines is estrogen. Estrogen levels fluctuate significantly during the menstrual cycle. It’s these fluctuations, particularly the drop in estrogen just before menstruation, that are believed to trigger migraines in susceptible individuals. Understanding the role of estrogen is crucial in identifying the triggers and potential treatment options for hormonal migraines.
The Menstrual Cycle and Migraines: A Complex Relationship
Phases of the Menstrual Cycle
To understand how the menstrual cycle impacts migraines, we need to break down the cycle into its four main phases:
- Menstrual Phase: This is the start of the cycle, marked by menstruation. Estrogen and progesterone levels are at their lowest.
- Follicular Phase: After menstruation, estrogen levels begin to rise as the body prepares for ovulation.
- Ovulation: Mid-cycle, estrogen peaks, triggering the release of an egg from the ovary.
- Luteal Phase: Post-ovulation, estrogen levels initially remain high but then drop sharply if pregnancy does not occur, leading to menstruation.
How Each Phase Affects Migraines
- Menstrual Phase: Low estrogen levels can trigger migraines in those sensitive to hormonal changes.
- Follicular Phase: Rising estrogen levels may provide some relief, but the upcoming ovulation can be a trigger point.
- Ovulation: The peak in estrogen can sometimes lead to migraines due to sudden hormonal changes.
- Luteal Phase: The drop in estrogen towards the end of this phase is a common trigger for migraines, often leading to what is termed as “menstrual migraines.”
Other Hormonal Triggers: Pregnancy, Menopause, and Contraceptives
Pregnancy
During pregnancy, estrogen levels remain consistently high, which can either exacerbate or alleviate migraine symptoms. Some women experience relief from migraines during pregnancy, while others may find their migraines worsen, especially during the first trimester.
Menopause
Menopause brings about significant hormonal changes, particularly a decrease in estrogen. This can lead to an increase in migraines for some women. However, post-menopause, when hormone levels stabilize, many women find relief from migraines.
Hormonal Contraceptives
The use of hormonal contraceptives can also impact migraines. Some women may experience an increase in migraines due to the hormonal changes induced by these contraceptives, while others may find relief. It’s a highly individual response and requires careful management and consultation with a healthcare provider.
Diagnosing Hormonal Migraines: The Importance of Tracking and Testing
Keeping a Migraine Diary
One of the most effective ways to diagnose hormonal migraines is to keep a detailed migraine diary. Tracking the timing, severity, and triggers of your migraines in relation to your menstrual cycle can provide invaluable insights. Note any patterns or recurring themes that could indicate a hormonal link.
Medical Tests and Evaluations
In addition to a migraine diary, medical tests such as hormone level evaluations can help diagnose hormonal migraines. Blood tests to measure estrogen and progesterone levels at different points in your cycle can provide a clearer picture of how your hormones may be influencing your migraines.
Treatment Options: From Lifestyle Changes to Medical Interventions
Lifestyle Modifications
- Diet: Certain foods and beverages can trigger migraines. Maintaining a balanced diet and avoiding known triggers such as caffeine, alcohol, and processed foods can help.
- Exercise: Regular physical activity can help regulate hormones and reduce the frequency and severity of migraines.
- Stress Management: Techniques such as yoga, meditation, and deep-breathing exercises can help manage stress, a common migraine trigger.
Medical Treatments
- Hormone Therapy: For some women, hormone therapy can help stabilize estrogen levels and reduce migraine frequency. This can include estrogen patches or contraceptives.
- Medications: Triptans, nonsteroidal anti-inflammatory drugs (NSAIDs), and other medications can be effective in treating acute migraine attacks. Preventive medications may also be prescribed.
Innovative Approaches and Future Directions
Neuromodulation Devices
Emerging technologies such as neuromodulation devices, which use electrical or magnetic stimulation to alter nerve activity, are showing promise in the treatment of migraines, including hormonal migraines.
Personalized Medicine
As our understanding of hormonal migraines improves, there is a growing emphasis on personalized medicine. Tailoring treatments based on an individual’s hormonal profile, genetic predispositions, and specific triggers can lead to more effective management strategies.
Conclusion: Bridging the Knowledge Gap
Hormonal migraines are a complex and often misunderstood condition. By understanding the role of hormones, particularly estrogen, in triggering migraines, we can better diagnose and treat this condition. Keeping a detailed migraine diary, seeking medical evaluations, and exploring both lifestyle modifications and medical treatments are essential steps in managing hormonal migraines. As research continues to evolve, we can look forward to more personalized and effective treatment options, ultimately bridging the knowledge gap and providing relief to those affected by hormonal migraines.
Call to Action
If you or someone you know suffers from hormonal migraines, don’t hesitate to seek medical advice and explore the various treatment options available. Staying informed and proactive is key to managing this challenging condition. Share this blog with others to spread awareness and help bridge the knowledge gap surrounding hormonal migraines. Together, we can pave the way for better understanding and management of this debilitating condition.