Pregnancy is often seen as a time of joy and anticipation, but for many women, it also brings a host of physical changes and challenges. One such challenge is dealing with migraines. This blog aims to demystify the topic of “migraine grossesse” (migraine during pregnancy), providing vital information that expectant mothers may not even realize they need.
Introduction: Understanding Migraine During Pregnancy
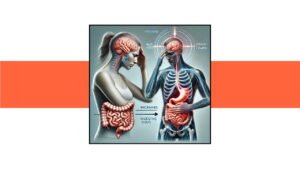
Migraines are intense headaches often accompanied by other symptoms such as nausea, vomiting, and sensitivity to light and sound. During pregnancy, the occurrence and management of migraines can be particularly complex due to hormonal changes and the need to consider the safety of both the mother and the unborn child.
The Unique Challenges of Migraine During Pregnancy
While migraines are challenging under any circumstances, pregnancy introduces additional factors that can exacerbate or alleviate symptoms. Understanding these unique challenges is the first step in managing migraines effectively during pregnancy.
The Prevalence and Impact of Migraines in Pregnancy
How Common Are They?
Migraines affect approximately 15-20% of women during their reproductive years, and many experience changes in migraine frequency and intensity during pregnancy. Some women may find their migraines improve during pregnancy, particularly in the second and third trimesters, while others may experience worsening symptoms.
The Impact on Daily Life
For expectant mothers, migraines can be particularly debilitating. The pain and associated symptoms can interfere with daily activities, including work and family responsibilities. Moreover, the stress and anxiety caused by frequent migraines can negatively impact both maternal and fetal well-being.
Hormonal Influences on Migraine During Pregnancy
The Role of Estrogen
Hormonal fluctuations are a key factor in the occurrence of migraines. Estrogen, a hormone that increases significantly during pregnancy, has a complex relationship with migraine. While some women experience relief from migraines due to stable high levels of estrogen, others may find that their migraines worsen, especially during the early stages of pregnancy.
Progesterone and Other Hormonal Changes
In addition to estrogen, other hormones like progesterone also play a role in migraine during pregnancy. Progesterone levels rise during pregnancy and can influence migraine patterns. Understanding these hormonal influences can help expectant mothers anticipate and manage their migraines better.
Triggers and Warning Signs
Common Triggers
Identifying and avoiding migraine triggers is crucial during pregnancy. Common triggers include:
- Stress: Emotional and physical stress can trigger migraines.
- Diet: Certain foods and beverages, such as chocolate, caffeine, and aged cheeses, can be triggers.
- Sleep Patterns: Irregular sleep, whether too much or too little, can provoke migraines.
- Environmental Factors: Bright lights, loud noises, and strong smells can be particularly problematic.
Recognizing Warning Signs
Understanding the early warning signs of a migraine can help in managing symptoms before they become severe. These signs may include:
- Aura: Visual disturbances such as flashing lights or zigzag patterns.
- Sensory Changes: Tingling or numbness in the face or limbs.
- Mood Changes: Irritability, depression, or euphoria.
Safe Management Strategies
Non-Pharmacological Approaches
Given the concerns about medication safety during pregnancy, non-pharmacological approaches are often the first line of treatment for managing migraines. These can include:
- Relaxation Techniques: Practices like yoga, meditation, and deep breathing can help reduce stress and prevent migraines.
- Dietary Adjustments: Avoiding known food triggers and maintaining a balanced diet can help manage symptoms.
- Hydration: Staying well-hydrated is essential, as dehydration can trigger migraines.
- Sleep Hygiene: Keeping a regular sleep schedule and ensuring quality sleep can reduce the frequency of migraines.
Safe Medications
When non-pharmacological approaches are insufficient, certain medications can be used safely during pregnancy under medical supervision:
- Acetaminophen: Often considered safe for use during pregnancy, it can help manage pain.
- Anti-Nausea Medications: These can be particularly useful if nausea and vomiting accompany the migraine.
It is crucial to consult with a healthcare provider before taking any medication to ensure it is safe for both the mother and the baby.
When to Seek Medical Help
Warning Signs
While migraines are typically not harmful to the pregnancy, certain warning signs should prompt immediate medical attention:
- Severe Headache: A sudden, severe headache that is unlike previous migraines.
- Neurological Symptoms: Symptoms such as vision loss, weakness, or difficulty speaking.
- High Blood Pressure: Persistent high blood pressure can be a sign of preeclampsia, a serious pregnancy complication.
Consulting a Specialist
For persistent or severe migraines, consulting a specialist such as a neurologist or a maternal-fetal medicine expert may be necessary. They can provide tailored advice and management strategies to ensure the well-being of both the mother and the baby.
Preparing for Delivery and Postpartum Period
Migraine Management During Labor
Planning for migraine management during labor is essential. Discussing pain management options with the healthcare team can help ensure a smooth delivery process.
Postpartum Considerations
After delivery, hormonal levels change rapidly, which can affect migraine patterns. New mothers should be prepared for potential changes and continue to use safe management strategies to cope with migraines during the postpartum period.
Conclusion: Empowering Expectant Mothers
Understanding and managing migraine during pregnancy requires a comprehensive approach that considers the unique hormonal and physiological changes occurring during this time. By identifying triggers, using safe management strategies, and seeking medical advice when necessary, expectant mothers can navigate this challenging aspect of pregnancy more effectively.
This blog aims to fill the information gap and empower expectant mothers with the knowledge they need to manage migraines during pregnancy. Remember, each pregnancy is unique, and it’s essential to consult with healthcare providers to develop a personalized plan that ensures the health and well-being of both the mother and the baby.