Migraines are notoriously debilitating, but did you know there is a specific type that can severely affect your vision? Welcome to the intricate world of “migraine ophthalmique,” a condition that often remains misunderstood and misdiagnosed. This blog aims to bridge that knowledge gap, providing you with a comprehensive understanding of migraine ophthalmique—its symptoms, causes, diagnosis, and treatment—through a structured learning curve.
What is Migraine Ophthalmique?
Migraine ophthalmique, also known as ocular migraine, refers to a type of migraine that predominantly affects the eyes. Unlike common migraines, which are primarily associated with severe headaches, migraine ophthalmique manifests through visual disturbances. These can include temporary loss of vision, blind spots, or seeing flashing lights. Interestingly, these visual symptoms can occur with or without the typical headache pain associated with migraines.
The Symptoms: More Than Meets the Eye
Understanding the symptoms of migraine ophthalmique is crucial in distinguishing it from other eye-related issues. Common symptoms include:
- Visual Aura: This is often the first sign of an impending migraine. Auras can present as shimmering or flickering lights, zigzag patterns, or blind spots in your vision.
- Scotomas: These are partial loss of vision or blind spots, typically occurring in the center of your visual field.
- Flashing Lights: Many sufferers report seeing bright, flashing lights, which can be distracting and disorienting.
- Temporary Vision Loss: In more severe cases, individuals may experience a temporary loss of vision in one eye, which can last from a few minutes to about half an hour.
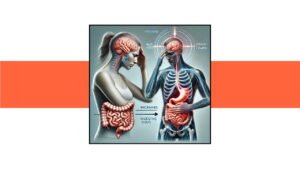
The Science Behind Migraine Ophthalmique
The exact cause of migraine ophthalmique remains elusive, but it is generally believed to involve the same mechanisms that trigger other types of migraines. Here’s a simplified breakdown:
- Genetic Predisposition: Migraines often run in families, suggesting a genetic component.
- Neurological Factors: Changes in brain activity can lead to a cascade of events affecting blood flow and nerve function.
- Vascular Changes: Fluctuations in blood flow to the brain and eyes can trigger visual symptoms.
- Environmental Triggers: Factors such as stress, lack of sleep, certain foods, and hormonal changes can precipitate an attack.
Diagnosing Migraine Ophthalmique: The Road to Clarity
Proper diagnosis of migraine ophthalmique is essential to differentiate it from other serious conditions like retinal detachment or stroke. The diagnostic process typically involves:
- Detailed Medical History: Your doctor will inquire about your symptoms, their frequency, and any family history of migraines.
- Eye Examination: A thorough eye exam helps rule out other eye-related issues.
- Neurological Examination: This may include tests to assess brain function and rule out other neurological disorders.
- Imaging Tests: In some cases, an MRI or CT scan may be ordered to rule out other potential causes of your symptoms.
Treatment and Management: Finding Relief
While there is no cure for migraine ophthalmique, several treatment options can help manage symptoms and reduce the frequency of attacks. These include:
- Lifestyle Modifications: Identifying and avoiding triggers, maintaining a regular sleep schedule, and managing stress can significantly reduce the frequency of migraines.
- Medication: Depending on the severity and frequency of your migraines, your doctor may prescribe medications. These can include pain relievers, anti-nausea medications, and preventive drugs such as beta-blockers, antidepressants, or anti-seizure medications.
- Alternative Therapies: Some individuals find relief through alternative treatments like acupuncture, biofeedback, and dietary supplements such as magnesium and riboflavin.
Living with Migraine Ophthalmique: Practical Tips
Living with migraine ophthalmique can be challenging, but these practical tips can help you manage your condition more effectively:
- Keep a Migraine Diary: Track your symptoms, triggers, and any treatments you try. This can help you and your doctor identify patterns and adjust your treatment plan accordingly.
- Adopt a Healthy Lifestyle: Regular exercise, a balanced diet, and adequate hydration can improve your overall well-being and reduce migraine frequency.
- Create a Relaxing Environment: Stress is a common trigger for migraines. Create a calm, relaxing environment at home and work to help manage stress levels.
- Stay Informed: Keep up-to-date with the latest research and treatment options for migraine ophthalmique. Joining support groups or online forums can also provide valuable insights and support from others who understand what you’re going through.
The Future of Migraine Ophthalmique Research
Research into migraine ophthalmique is ongoing, with scientists exploring new treatments and potential causes. Advances in neuroimaging and genetics are providing deeper insights into the mechanisms behind migraines, which could lead to more effective treatments in the future. Promising areas of research include:
- Neurostimulation Devices: These devices use electrical or magnetic pulses to modulate nerve activity and reduce migraine frequency.
- Monoclonal Antibodies: These are a new class of preventive medications that target specific proteins involved in the migraine pathway.
- Genetic Studies: Understanding the genetic basis of migraines could lead to personalized treatment approaches tailored to an individual’s genetic makeup.
Conclusion: Bridging the Knowledge Gap
Migraine ophthalmique may be less well-known than other types of migraines, but it can be equally disruptive to daily life. By understanding its symptoms, causes, diagnosis, and treatment options, you can take proactive steps to manage this condition and improve your quality of life. Remember, you are not alone—many people live with migraine ophthalmique, and ongoing research continues to shed light on this complex condition. Stay informed, stay proactive, and most importantly, take care of yourself.
By closing the knowledge gap about migraine ophthalmique, we can foster greater awareness and support for those affected by this challenging condition. If you suspect you may have migraine ophthalmique, consult with a healthcare professional to receive a proper diagnosis and develop a personalized treatment plan.